Cataract Surgery
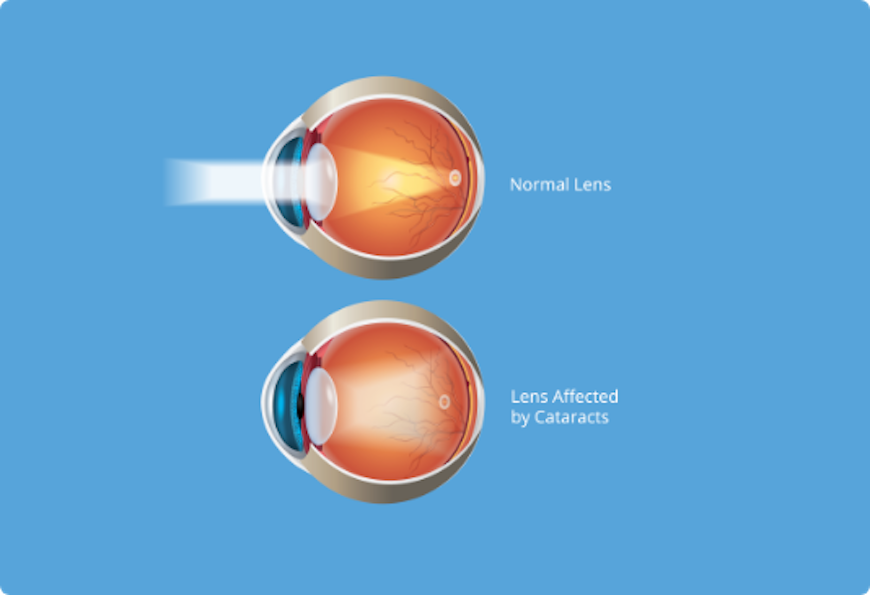
Cataract is a clouding of the eye’s lens. When we look at something, light rays travel into our eye through the pupil and are focused through the lens onto the retina, a layer of light-sensitive cells at the back of the eye. The lens must be clear in order to focus light properly onto the retina. If the lens has become cloudy, this is called a cataract.
Cataracts can occur at any age but it is mostly common in older people due to lenses metabolic disorders. In younger people it usually the result of injuries, use of the medications, or the result of general or eye diseases.
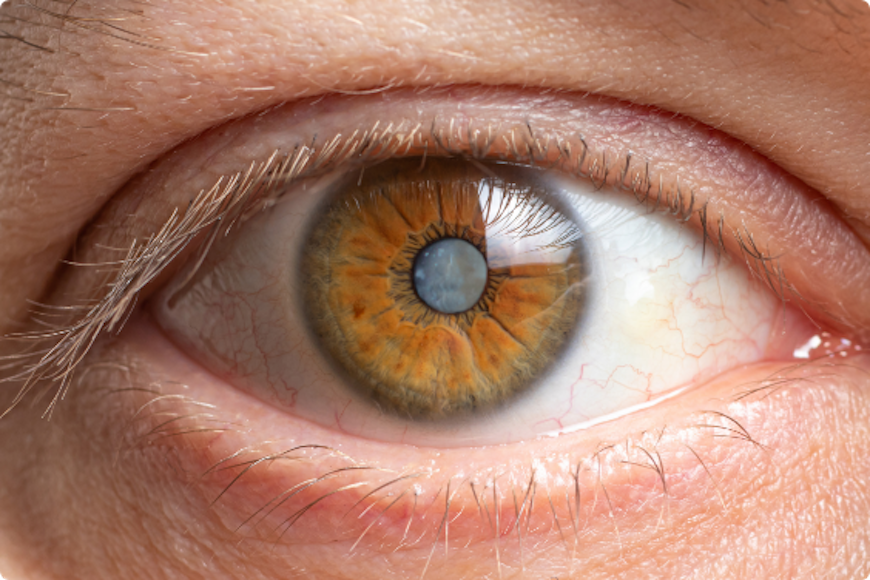
The degree of blurriness within the lens can vary. If blurring is not close to the centre of the lens you may not even be aware that a cataract is present.
Cataract Symptom Progression
- Painless cloudy, blurry or dim vision;
- More difficulty seeing at night or in low light;
- Sensitivity to light and glare;
- Seeing halos around lights;
- Faded or yellowed colors;
- The need for brighter light for reading and other activities;
- Frequent changes in eyeglass or contact lens prescription;
- Double vision within one eye.
Cataract is most frequently associated with aging. Diabetes, smoking, hereditary predispositions or long-term use of certain medicinal products may play a certain role.
If your vision is only slightly blurry, a change in your eyeglass prescription may be all you need for a while. However, after changing your eyeglass prescription, if you are still not able to see well enough to do the things you like or need to do, you should consider cataract surgery.
With cataract surgery, your eye’s cloudy natural lens is removed and replaced with a clear artificial lens implant (called an intraocular lens, or IOL). Your ophthalmologist will discuss the cataract surgery procedure, preparation for and recovery after surgery, the benefits and possible complications of cataract surgery and other important information.
How is the procedure performed?
The surgery is part of outpatient care, which means that you will return home on the same day. Prior to the procedure we will perform control measurements, and after their completion you will have local anesthetic drops applied in your eye to ensure a completely painless procedure, and pupil widening drops.
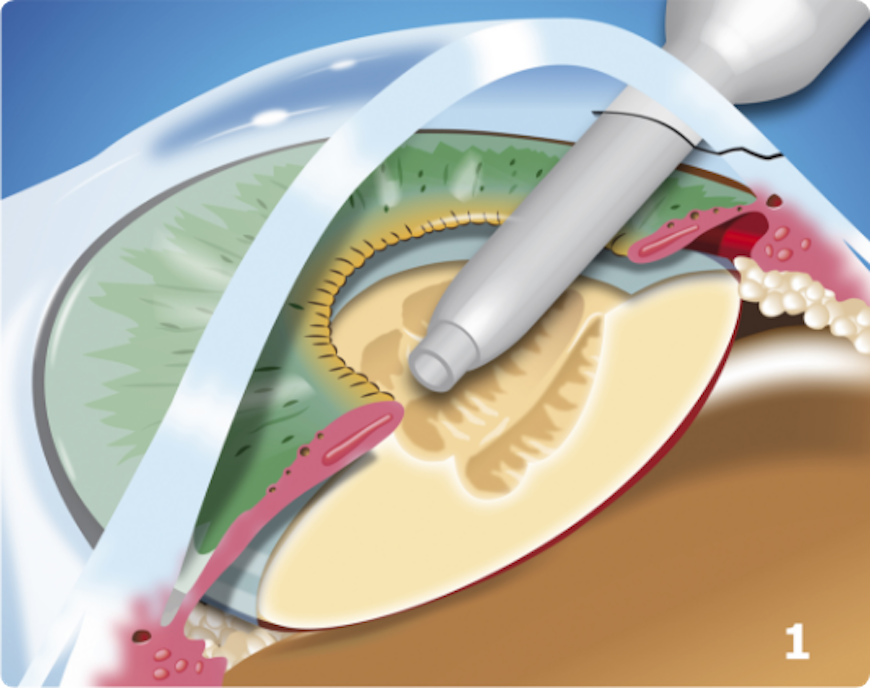
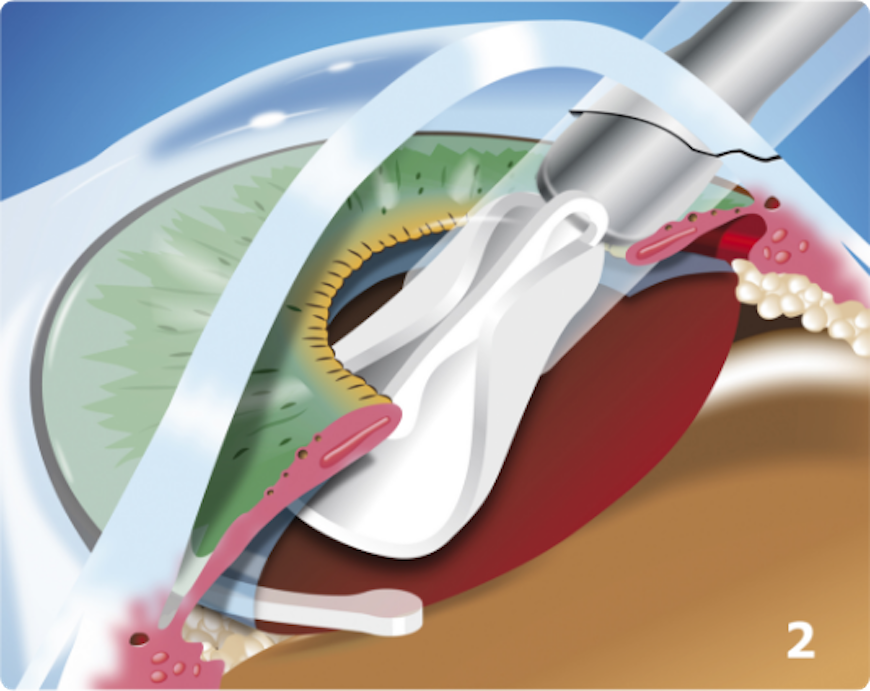
The most common procedure used for removing cataracts is called phacoemulsification. A small incision is made in the side of the cornea (the front part of your eye), where your Eye M.D. inserts a tiny instrument that uses high-frequency ultrasound to break up the center of the cloudy lens and carefully suction it out.
After the cloudy lens has been removed, the surgeon will replace it with an intraocular lens (IOL). The procedure takes approximately 15 minutes and is completely painless.

Cataract surgery recovery
You will spend a short period of time resting in the outpatient recovery area before you are ready to go home. You will need to have someone drive you home.
Following your surgery, it is very important to put in the eye drops exactly as prescribed by your ophthalmologist to promote healing. You will also need to take care to protect your eye by wearing the eye shield whenever you sleep, and by wearing special wraparound sunglasses in bright light. Be sure not to rub your eye.
During the first week of your recovery, you must avoid strenuous activity such as exercise or bending and heavy lifting (including anything over 25 pounds). You will also need to avoid getting any water, dirt or dust in your eye, which can lead to infection.
Glasses are prescribed after a few weeks.
When will you go back to work depends on your profession and for this it is necessary to consult an ophthalmologist.
Cataract surgery risks and complications
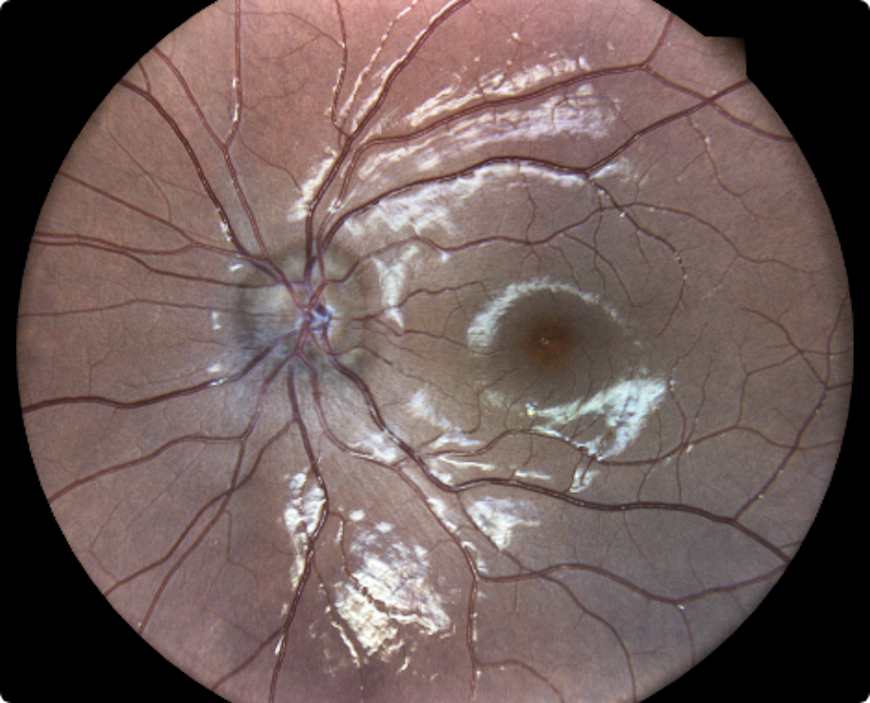
As with any surgical procedure, there are risks associated with cataract surgery. Complications during cataract surgery are rare and occur in 1-2% of cases. They can be solved in most of the rimes with eye drops or other drugs, but it is not excluded the need for a subsequent intervention or surgery. The serious complications of cataract surgery, which can threaten vision include: corneal clouding, separation of the retina (retinal detachment) which results in about 1% of cases, severe internal bleeding in the eye (1-2 per 1000 cases), infection, endophthalmitis (1 in 1000 cases).
Also is possible: changes in shape of the pupil, the iris damage, change in position of the eyelids, glaucoma, intraocular lens dislocation, pain or other unpleasant sensations in the eye. The postoperative complications include non-infectious inflammatory reaction, and swelling of the retina (cystoid macular oedema).
One of the most common cataract surgery complication is a posterior capsule opacity (also called posterior capsule opacification or PCO). In about 20 percent of patients, the posterior portion of the capsule becomes hazy some time during cataract surgery recovery or even months later, causing PCO. Posterior capsule opacification occurs because lens epithelial cells remaining after cataract surgery have grown on the capsule. Fortunately, a YAG laser can treat posterior capsule opacity safely, effectively and painlessly. This procedure, known as YAG laser capsulotomy, often can be performed in your doctor’s office.
Risks of delays and cancellation of cataract surgery
Standard cataract is not urgent indication for surgery and it is planned depending on the degree of visual impairment and needs of each individual patient. However, in case of long delays it is possible that the surgery becomes complicated and risky due to hardening and full opacification of the lens. Rarely, it can happen that an untreated cataract causes glaucoma attack or very bad eye inflammation that can lead to permanent visual impairment.

