What is Keratoconus
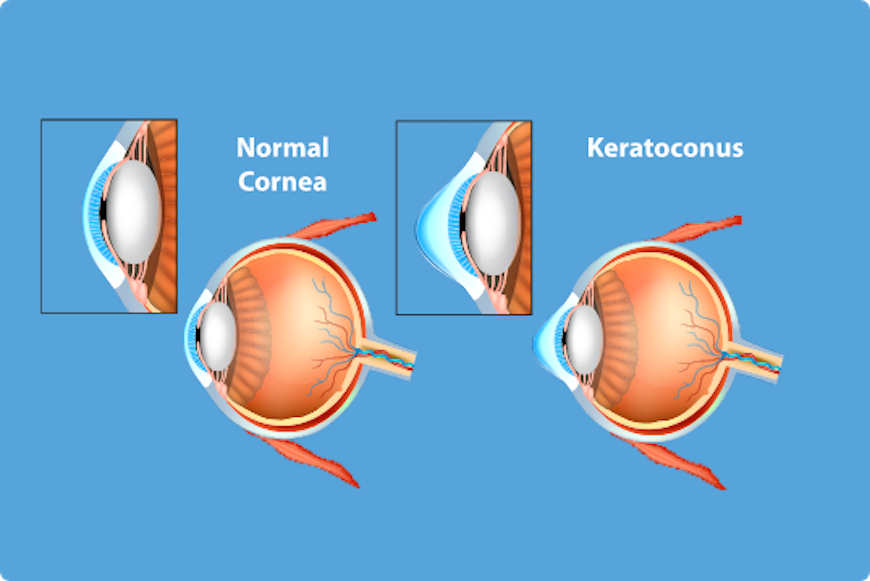
Keratoconus is degenerative disease that is manifested through cornea curvature disorder. This disease makes cornea thinner and makes a little bump to like a cone and therefore, creates vision difficulties. The base of this problem is defect of collagen fiber, basic part of cornea structure.
This disease is always bilateral (affects both eyes) where one eye is more affected than the other. Keratoconus is progressive disease which end case requires cornea transplantation.

Keratoconus is disease that appears among young children and youth, usually appearing form the age of 16. It develops much faster in early childhood and puberty. Progress is fastest in afirst 10-15 years, and then there is little slower development. It rarely occurs after the age of 40.
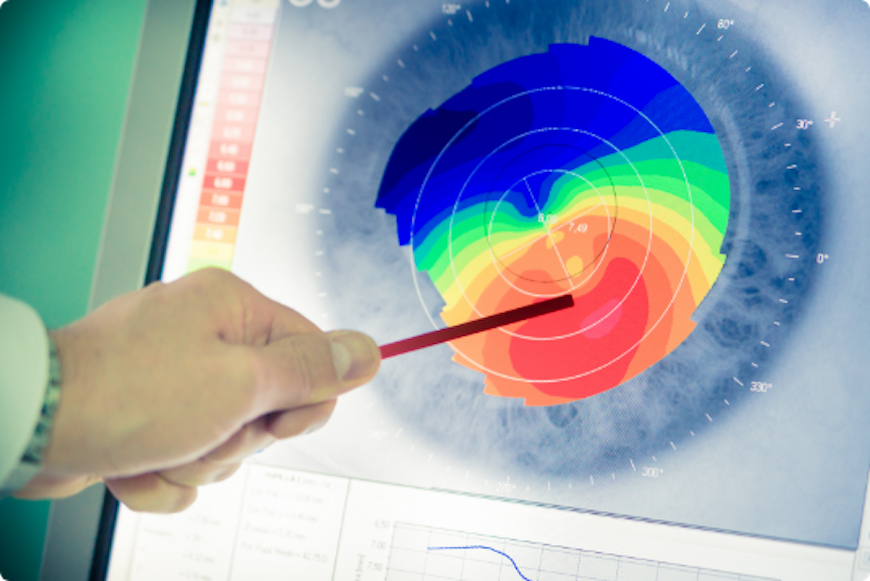
The method that diagnoses keratoconus for sure is corneal topography. This method gives all important diagnostic details as well as tracking the progress of keratoconus (cornea thickness, curvature, existence or non-existence of a bump on both front and back side of cornea, stage of the keratoconus). Close attention needs to be paid to the existence and early discovery of “forme fruste” keratoconus which is a subclinical form and cannot be discovered in any other way. This is the earliest stage that does not show any typical symptoms and signs that are seen in already developed and clinically seen keratoconus. One characteristic of corneal topography is normal finding on the font side of cornea, combined with abnormal bump of the back side that is over 15 micrometers.
What are keratoconus symptoms?
Basic symptom of keratoconus patients is vision clarity impairment. There is no redness or pain, but higher sensitivity to light and feeling of light scattering are possible. There can be difficulties driving at night. Diopter grows quickly, especially the cylindrical component. Typically, this is myopic astigmatism.
Through normal human eye, light rays diffract at the entrance through two curvy surfaces, through cornea and lens. Normal cornea has round shape like a hemisphere. Light rays diffract through cornea that directs them through lens further in the eye and all rays intersect exactly on retina. This produces clear image.
If there is keratoconus, cornea does not have normal round shape, it has a bump. Rays that fall on cornea diffract through it and are not correctly directed through the eye so they don’t intersect exactly on retina. Rays are scattered and image is not clear and blurry.
Keratoconus phases
Keratoconus has four phases:
- Phase I: there is myopic astigmatism that can be corrected relatively good using eyeglasses. In most cases, disease is not discovered and it is treated as a refractive disorder.
- Phase II: dioptre increases, especially cylindrical component. Eyeglasses don’t help achieve wanted vision clarity. Gas permeable (GP connect) contact lenses are used then which help achieve clear vision.
- Phase III: Disease grows even more, vision clarity reduces, RGP lenses become uncomfortable, and they cannot be worn the whole day and fall out of the eye easily.
- Phase IV: This phase is characterized by the appearance of a scar on the thinnest part of cornea which additionally worsens vision. Cornea is very thin and bumpy, lens falls out of the eye because by blinking. In this situation, cornea transplantation is considered.
Main factors that help keratoconus grow are: age, constant rubbing of the eyes, and pregnancy. The earlier this disease occurs, faster it grows and more progressive it is so regular tracking is necessary. Considering that this disease is inheritable, special attention is required for patients whose relatives have keratoconus.
How to treat keratoconus?
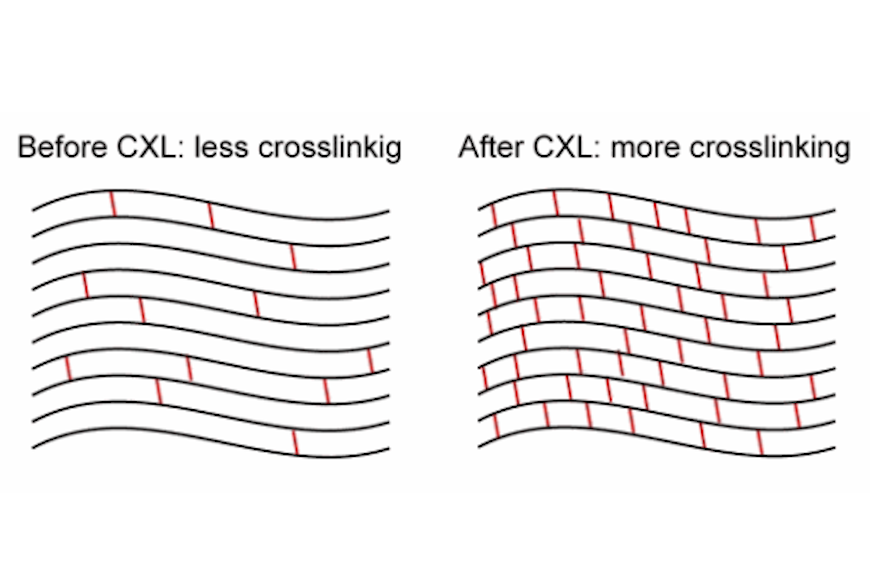
Not so long ago, the only way of treating keratoconus patients was keratoplasty which is cornea transplantation. Since the discovery of corneal cross linking procedure, in most cases it is possible to stop keratoconus progress before it significantly develops and vision reduces drastically. This short and unpainful surgical intervention stops further development of keratoconus. It is unaggressive therapy using vitamin B2 and UV rays (ultra B2 or CXL) that strengthens collagen and stabilizes cornea, stops cornea from getting thinner and bumpier, and that way stops keratoconus development.
Vitamin B2 is biocompatible substance which structure absorbs ultraviolet light, creates new bond with collagen in stromal layer of cornea which leads to stronger mechanic force in cornea itself, while not affecting its transparency.
New method strengthens cornea, disabling further deformation
Professor Theo Seiler came up with this method and was first one to use it in 1997. He got the idea of finding matter that would strengthen cornea and stop keratoconus from his dentist. White paste that is put into a tooth strengthens under ultraviolet light and creates tooth filling. Professor used this to find matter that would be transparent and would be able to strengthen cornea under ultraviolet light – so he found vitamin B2.
Ultra B2 intervention lasts about half an hour and it is done with local anaesthesia (anaesthetic drops). Thin surface layer of epithelium is removed, cornea’s protection layer. Vitamin B2 is placed in form of drops and it is left like that for about 20 minutes to enable penetration of the vitamin B2 throughout whole cornea.
It is then put under ultraviolet light for 3 to 30 minutes, depending on the lamp power with constant use of vitamin of B2 and anaesthetic.
Procedures ends with placements with special therapeutic lens which role is to protect the eye while epithelium heals, after which this lens is removed (up to 7 days).
Post-surgical treatment
After the surgery keratoconus should be stopped at the level it was. Although the goal of the surgery is to stop further development of keratoconus, lately research shows that it is possible to improve vision clarity to a certain level depending on the stage keratoconus is at. Eye drop treatment after the surgery is required for several months with regular check-ups. Patient can keep wearing contact lenses for about month or two after the intervention. Seven to ten days after the surgery, the pre-intervention state is established again. Ultra B@ can be used for other corrections as well i.e. Ferrara rings implantation.
Recently, very significant is combined procedure that includes simultaneous use of CXL (cross linking) and PRK methods for dioptre correction that is at a certain level, primarily astigmatism together with cornea strengthening. This method is widely used today with patients that have mild to moderate level of keratoconus. This helps strengthen cornea as well as improve vision clarity. That is why it is very important to discover keratoconus early while cornea has certain thickness and it is possible not only to strengthen cornea but to partially correct dioptre as well. Combined procedure is mostly used for “forme fruste” keratoconus.

In some cases, cross linking method is recommended as prophylactic when cornea is thin and LASIK or PRK methods are planned even though keratoconus is not diagnosed. It should be mentioned that this method alone or in combination with others has certain risks and results can be sometimes limited and unpredictable. However, complication percentage is not significant compared to success rate and significance of this method. Besides keratoconus, cross linking method is used for stopping the progress of pellucid marginal degeneration, ecstasies after refractive procedure, for treating state that melts cornea (melting conditions) and for infective keratitis where cornea is also getting strengthen while UV rays sterilize infective matter.
Cross linking is a “gold standard” today in stopping keratoconus progression, ecstasy and pellucid marginal degeneration. This revolutionary discovery is considered one of the biggest inventions in modern ophthalmology.
Other treatment methods
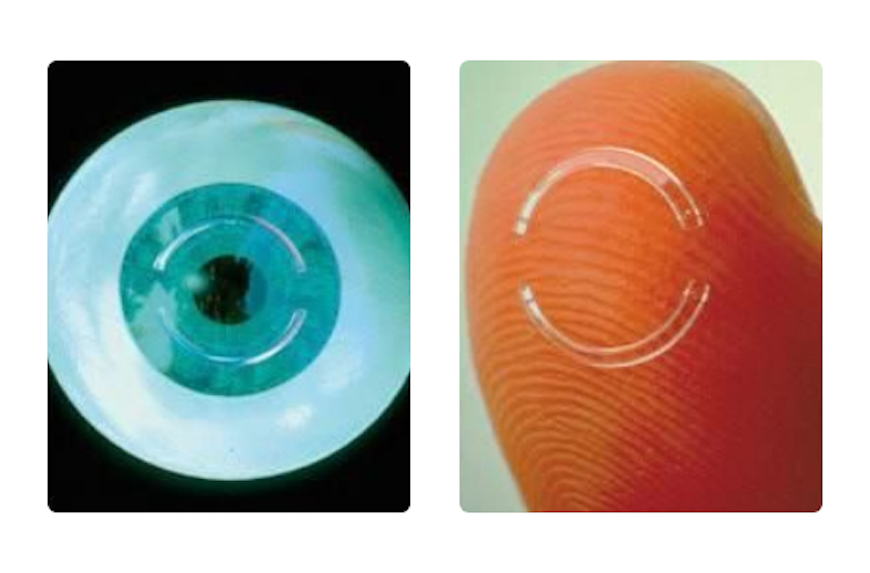
Corneal stromal ring implantation
- This represents alternative cornea transplantation.
- The method consists of intrastromal ring implantation into the cornea middle periphery. Central part becomes flattened and more regular which reduces myopia, especially astigmatism, and increases vision quality.
- This implantation lasts about fifteen minutes with local anaesthesia (anaesthetic drops). Special spatulas are used to make a “hall” in deeper cornea levels in which one or two semi rings are implanted.
- Protective contact lens is placed on the eye instead of the bandage until the following day, and use of postsurgical eye drops is necessary for several weeks after the intervention.
Most known intrastromal rings are Intacs and Ferrara Rings.
Cornea transplantation
Between 10 and 25% of untreated keratoconus cases develop to a stage where vision correction is not possible anymore because cornea is too thin and has scars. In this cases cornea transplantation is necessary. Damaged, curved, blurred, or cornea with scars is replaced with healthy donated one. In case of keratoconus there are two methods: DALK and perforating keratoplasty PKP. Depending on the place of pathological changes in cornea in regards to cornea thickness, transplantation can be:
- Full cornea thickness transplantation – perforating keratoplasty
- Partial cornea transplantation – lamellar keratoplasty
- Using DALK method, only outside epithelium and stroma are replaced which enables cornea’s back side to stay in the eye and keep structural integrity and stability. Since graft replacement starts in endothelial part, there are small chances for this are very small with this type of transplantation. Advantages in regards to PKP are: extra ocular procedure, keeping back part of cornea, quicker recovery. Disadvantages are: more complicated to do, more complications during surgery.
The most important thing is NOT TO LET keratocnus develop to transplantation stage. Today there is way to successfully fight and prevent significant keratoconus progression and vision impairment caused by it. Early discovery of this disease, regular check-ups and timely use of cross linking method are crucial in achieving good results.

