What is retina?
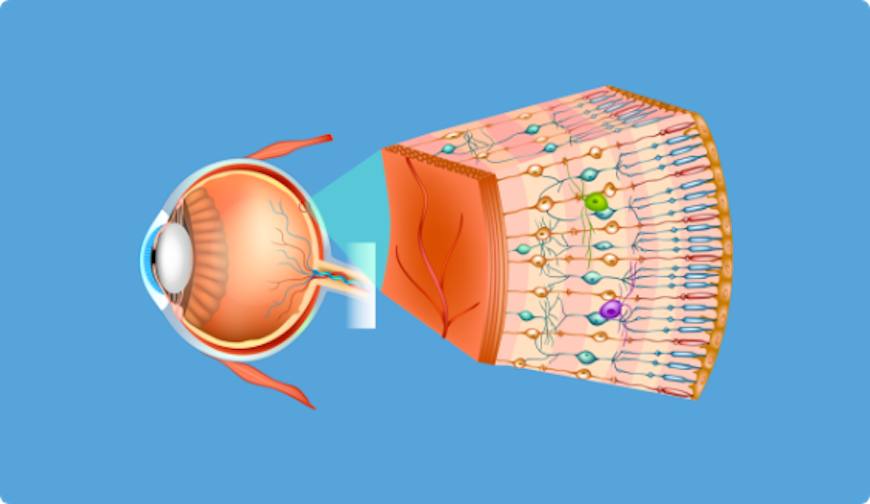
The retina is a layer of nerve tissue inside the eye that is sensitive to light and sends images to the brain.
The eye is like a camera. The cornea and the lens at the front of the eye focuses light on the retina. You can imagine the retina as the film that lines the back of the camera.
 `
`
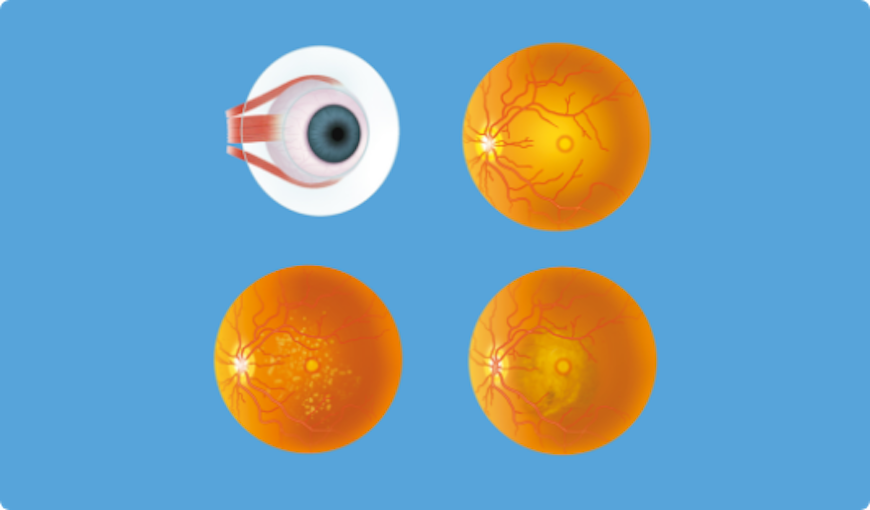
What is macula?
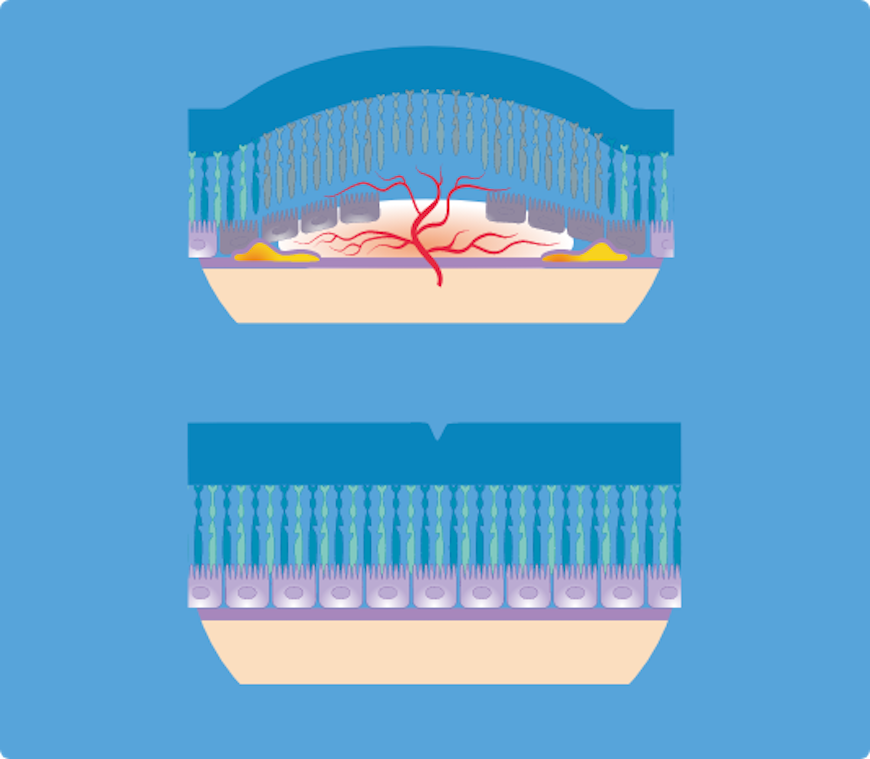
Macula represents the point of focus. It is a part of retina which, thanks to its specific structure, allows us to see fine details clearly and to do things such as reading and driving. When macula does not function properly, our central vision can be blurred, distorted or only be a dark spot.
What is vitreous?
Vitreous is a transparent gel that fills the central part of the eye. With aging, the gel is slowly turning into the water and can be separated from the retina in the back of the eye.
Typically, the gel is separated from the retina without causing any complications.
But sometimes this separation can cause certain complications:
- The occurrence of the retinal rupture (tear of the retina in one or more places)
- Retinal detachment (retinal tear as a result of rupture of the retina).
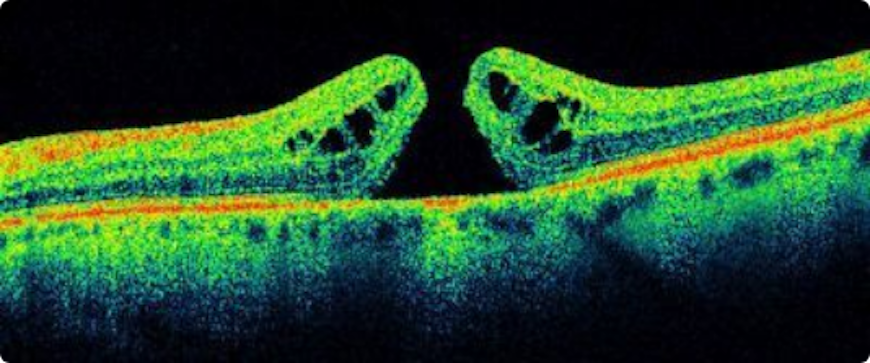
- The occurrence of holes in the macula
- The occurrence of folds in the macula
- Hemorrhages within the eye
- The appearance of Weiss ring, which presents the visible involucre of the vitreous body.
It often interferes with vision and the patient has the appearance of “flies”, “circle”, “crescent” or black spots in the visual field. Usually this change is harmless, but its occurrence requires a detailed review of the fundus periphery.
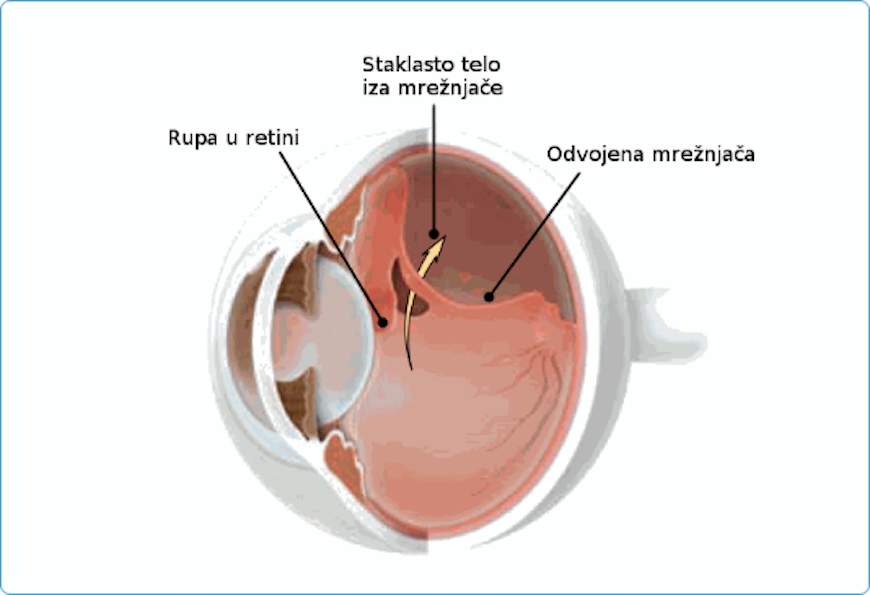
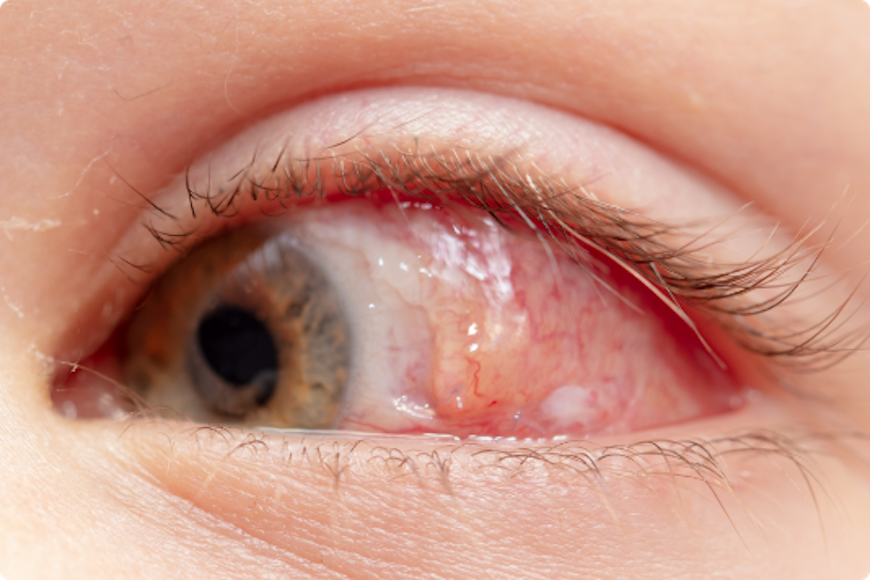
What is retinal detachment (retinal tear)?
Usually, the vitreous moves away from the retina without causing problems. But sometimes the vitreous pulls hard enough to tear the retina in one or more places. Fluid may pass through a retinal tear, lifting the retina off the back of the eye.
When the retina is pulled away from the back of the eye like this, it is called a retinal detachment.
The retina does not work when it is detached and vision becomes blurry. A retinal detachment is a very serious problem that almost always causes blindness unless it is treated.
People with the following conditions have an increased risk for retinal detachment:
- Nearsightedness;
- Previous cataract, glaucoma or other eye surgery;
- Glaucoma medications that make the pupil small (like pilocarpine)
- Severe eye injury;
- Previous retinal detachment in the other eye;
- Family history of retinal detachment;
Weak areas in the retina that can be seen by an ophthalmologist during an eye exam.
Retinal Detachment; Torn or Detached Retina Symptoms
Symptoms of a retinal tear and a retinal detachment can include the following:
- A sudden increase in size and number of floaters, indicating a retinal tear may be occurring;
- A sudden appearance of flashes, which could be the first stage of a retinal tear or detachment;
- Having a shadow appear in the periphery (side) of your field of vision;
- Seeing a gray curtain moving across your field of vision;
- A sudden decrease in your vision.
Floaters and flashes in themselves are quite common and do not always mean you have a retinal tear or detachment. However, if they are suddenly more severe and you notice you are losing vision, you should call your ophthalmologist right away.
Retinal Detachment: Torn or Detached Retina Treatment
A retinal tear or a detached retina is repaired with a surgical procedure. Based on your specific condition, your ophthalmologist will discuss the type of procedure recommended and will tell you about the various risks and benefits of your treatment options.
Torn retina surgery
Most retinal tears need to be treated by sealing the retina to the back wall of the eye with laser surgery or cryotherapy (a freezing treatment). Both of these procedures create a scar that helps seal the retina to the back of the eye. This prevents fluid from traveling through the tear and under the retina, which usually prevents the retina from detaching.
Laser surgery (photocoagulation)
With laser surgery, your ophthalmologist uses a laser to make small burns around the retinal tear. The scarring that results seals the retina to the underlying tissue, helping to prevent a retinal detachment.
Freezing treatment (cryopexy)
Your eye surgeon uses a special freezing probe to apply intense cold and freeze the retina around the retinal tear. The result is a scar that helps secure the retina to the eye wall.
Detached retina surgery
Almost all patients with retinal detachments must have surgery to place the retina back in its proper position. The method for fixing retinal detachment depends on the characteristics of the detachment. In each of the following methods, your ophthalmologist will locate the retinal tears and use laser surgery or cryotherapy to seal the tear.
Scleral buckle This treatment involves placing a flexible band (scleral buckle) around the eye to counteract the force pulling the retina out of place. The ophthalmologist often drains the fluid under the detached retina, allowing the retina to settle back into its normal position against the back wall of the eye. This procedure is performed in an operating room.
Pneumatic retinopexy
In this procedure, a gas bubble is injected into the vitreous space inside the eye in combination with laser surgery or cryotherapy. The gas bubble pushes the retinal tear into place against the back wall of the eye. Sometimes this procedure can be done in the ophthalmologist’s office. Your ophthalmologist will ask you to constantly maintain a certain head position for several days. The gas bubble will gradually disappear.
Vitrectomy
This surgery is commonly used to fix a retinal detachment and is performed in an operating room. The vitreous gel, which is pulling on the retina, is removed from the eye and usually replaced with a gas bubble.
When you need vitrectomy?
Your ophthalmologist (eye doctor) may recommend a vitrectomy in order to treat following complications
- detachment of the retina,
- post-traumatic conditions,
- changes on the retina in diabetes – proliferative diabetic retinopathy,
- ailments of the macula – macular hole,
- macular pucker.
Vitrectomy – surgery
The surgery duration ranges from one to several hours, depending on your situation. In certain situations, your ophthalmologist can simultaneously perform another surgical procedure such as a correction of detached retina or removing a cataract.
Your ophthalmologist performs the surgery while looking at your eye with a microscope. Various miniature instruments are placed into the eye through a small incision in the sclera (white part of the eye). Cut size depends on the equipment used for the operation. Nowadays, in most cases in use is a technique with a very small incision which does not need stitches and due to that the wound closes itself. Clinic Maja has the latest medical equipment so that procedure is carried out with a small incision, so called micro incision vitreo retinal surgery.
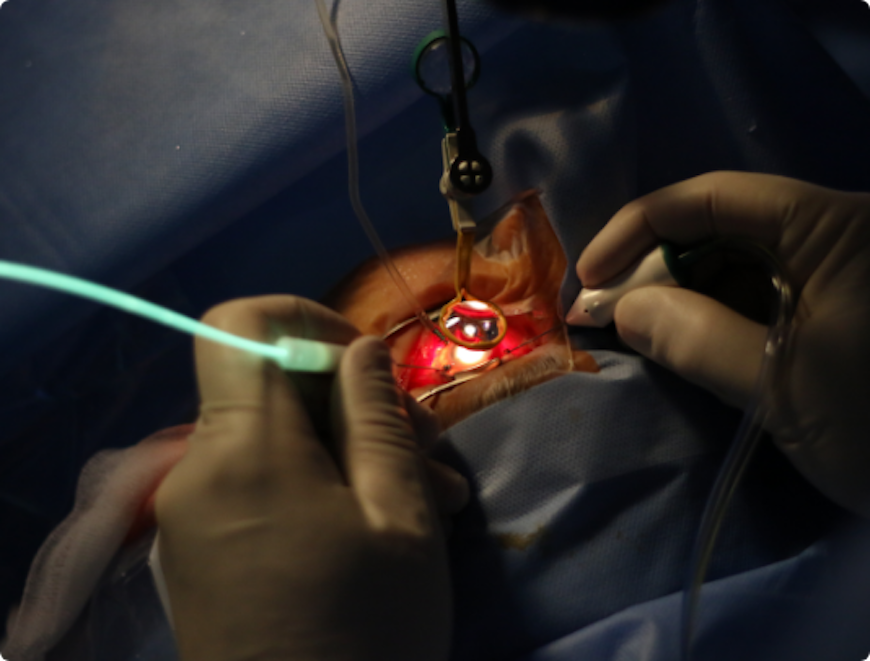
To bring you the best possible vision, your ophthalmologist will do one or more of the following:
- Will remove all blurring in the vitreous body;
- Will remove all existing damaged tissue, trying to return the retina to its natural position;
- Will remove the foreign body that may be in the eye;
- Will use the laser in the treatment of the eye in order to reduce future bleeding or to correct tear in the retina.
- Will inject nozzle air or other gas bubble into the eye so that retina retained its natural position, depending on the gas used 7 days to 2 months is required to gas bubble to gradually disappear from the eye. During the disappearance of the gas from the eye sight gradually occurs, the first image appears in the upper part of the visual field.
- Will inject oil bubble in the eye that usually must be later removed surgically.
Sometimes an oil bubble is used (instead of a gas bubble) to keep the retina in place. Your body’s own fluids will gradually replace a gas bubble. An oil bubble will need to be removed from the eye at a later date with another surgical procedure. Sometimes vitrectomy is combined with a scleral buckle.
You can expect some inconvenience after surgery. Your ophthalmologist will prescribe the necessary medication and tell you when you can resume your normal activities. You will need to wear a bandage over one eye for a shorter period.
Do not fly in an airplane or travel at high altitudes until you are told the gas bubble is gone. A rapid increase in altitude can cause a dangerous rise in eye pressure. With an oil bubble, it is safe to fly on an airplane.
Vitrectomy – surgery risks
Each surgery carries certain risks, but in vitrectomy risks are lower compared to the expected improvement in vision.
Some of the vitrectomy risks include:
- Infection;
- bleeding:
- Retina detachment;
- Poor (bad) vision;
- High eye pressure
Will your vision improve?
Most retinal detachment surgeries (80 to 90 percent) are successful, although a second operation is sometimes needed.
Some retinal detachments cannot be fixed. The development of scar tissue is the usual reason that a retina is not able to be fixed. If the retina cannot be reattached, the eye will continue to lose sight and ultimately become blind.
The more complicated the situation on the eye ground (advanced changes from diabetes, a hole in the macula that is long present, the old retinal detachment with scar changes …), the smaller the percentage of vision can be saved.
Therefore, it is very important to contact your eye doctor immediately if you notice any problems.

